Benjamin Tan Kye Jyn, an NUS alumnus and House Officer at the National University Hospital, has always been drawn to the medical sciences. But it was the chance to make a difference in people's lives that truly fuelled his passion for becoming a doctor.
“I was drawn to the field of medicine by its heart and soul — the opportunity to care for patients in their most vulnerable moments.”
Driven by this desire, he decided to embark on a life-changing journey as a medical student at the NUS Yong Loo Lin School of Medicine (NUS Medicine).
At the cutting edge of medicine
NUS Medicine prepares its students to become tomorrow's visionary healthcare leaders by ensuring that they gain a broad understanding of the entire medical industry and its many moving parts.
“NUS houses students from various healthcare and related professions, such as nursing, pharmacy, dentistry and social work. So we have opportunities to interact and learn from each other, whether through school-organised interprofessional education, or via ground-up community service initiatives. After starting work, I’ve realised how important it is that we work together to care for patients holistically.”
 Benjamin (first from right) enjoyed spending time with his clinical groupmates.
Benjamin (first from right) enjoyed spending time with his clinical groupmates.
The initial years of the NUS Medicine curriculum are designed to set the foundation for students to understand fundamental medical principles. “The first two years were grade-free, so we were able to focus a lot more on the learning, without experiencing unnecessary academic stress,” he adds.
Other exciting developments included advanced simulations and immersive virtual reality (VR) experiences that were used to enhance their learning.
"Throughout our years in medical school, and especially in our final year, our school used realistic simulation equipment, mannequins and team-based scenarios to train us as doctors. We had two full weeks in our final year focused on advanced cardiac life support and critical care scenarios, where we trained at NUS Medicine’s Centre for Healthcare Simulation under Prof Suresh Pillai and his team,” Benjamin shares.
“These realistic simulations were incredibly helpful when I encountered cardiac arrests and other emergencies after starting work.”
NUS Medicine is also developing cutting-edge VR technology to train its students in anatomy and surgical skills. “We’ve had the opportunity to use devices like the Oculus Rift to visualise anatomy in 3D. These virtual environments were built in-house by our school’s software engineers. It’s fun and immersive, and even funnier when you take off the headset and watch your friends bumble around," Benjamin recounts with a smile.
He also highlights the benefits of using VR for learning during the COVID-19 pandemic: "To avoid exposing us to COVID-19 at the peak of the pandemic, we were given less patient contact, including less time in the operating theatres. I recall a VR surgery course that our school created to help us learn as best as we could, despite the restrictions.”
He also credits his teachers for ensuring a smooth transition to remote learning during the height of COVID-19 restrictions. Prior to the pandemic, lectures and tutorials were decentralised and organised by each hospital separately during postings. Benjamin’s batch, however, had centralised classes on Zoom, which he believes to have prepared them better for their postings. They often had half-day clinical postings and half-day online tutorials as part of a hybrid arrangement. The school’s adaptations, Benjamin noted, created a “lasting impact” due to the increased support they felt from the tutors.
“The school really did an amazing job in adapting. All of the tutors banded together. They were working overtime to redesign the whole curriculum for COVID-19 — and it turned out to be better!”
Exploring the wards
In Year 3, medical students gradually transition to become members of the healthcare teams in hospitals, where they are rotated through different departments, so that they can gain exposure to as many specialties as possible.
 Benjamin (second from left) and fellow NUS Medicine students, Jonathan Chua, Cowan Ho, Chong Kai Ning, Celene Ng and Sophie Tan (who was digitally added into the group picture as she was on Stay Home Notice when this photo was taken) on their clinical posting at the Accident & Emergency department at Changi General Hospital.
Benjamin (second from left) and fellow NUS Medicine students, Jonathan Chua, Cowan Ho, Chong Kai Ning, Celene Ng and Sophie Tan (who was digitally added into the group picture as she was on Stay Home Notice when this photo was taken) on their clinical posting at the Accident & Emergency department at Changi General Hospital.
“In my third year, I was posted to Internal Medicine at Changi General Hospital as one of my four postings. Every week, I was rotated to a different team, which allowed me to experience the breadth of medicine,” Benjamin recalls, adding that he worked alongside medical teams which specialised in conditions related to the heart, lungs, stomach and kidneys, as well as organ and blood cancers.
Although the COVID-19 restrictions implemented in Singapore in 2020 and 2021 coincided with Benjamin's third and fourth years of medical school, he was keen to get the most out of his learning experience regardless of the circumstances.
“In our fourth year, some of our postings were compressed from 6 weeks to just 2 weeks,” Benjamin remembers. But instead of letting these obstacles hinder their progress, Benjamin and his classmates embraced the challenge and worked harder and faster to make the most of their time at the hospitals.
He explains: "We didn't let these setbacks slow us down. We learned to be resourceful and to make the most of every opportunity. And in the end, we all succeeded in making our time at the hospitals as enriching as possible, with the strong support of our tutors."
Diagnosing the road ahead
At NUS Medicine, Benjamin was given many opportunities to uncover his passion for research.
"Not everyone likes research, but I found it incredibly rewarding," Benjamin said. "It gave me the opportunity to make a difference on a larger scale, rather than (helping) just one person at a time."
Throughout his time at NUS, Benjamin completed and published over 30 research projects in peer-reviewed journals, with close to 400 citations to date. Although he initiated many of his research projects independently, he could rely on NUS’ network of research professionals and nurturing mentors who were always willing to extend a helping hand.
“I was very fortunate to have met mentors who guided me, and who connected my friends and I to researchers with ongoing studies. Innovation happens at the boundaries of disciplines, and NUS Medicine has an excellent environment for fostering collaborations.”
One of his most notable projects involved studying the recovery of a patient’s sense of smell and taste following a COVID-19 infection, where he took on the role of first author under the able mentorship of Associate Professor Toh Song Tar from Singapore General Hospital’s Ear Nose & Throat Department.
 Benjamin (second from left) enjoying a meal with Associate Professor Toh Song Tar (first from left) and Dr Anna See (first from right), who was also part of the project.
Benjamin (second from left) enjoying a meal with Associate Professor Toh Song Tar (first from left) and Dr Anna See (first from right), who was also part of the project.
The team used a statistical method called "cure modelling" to project the number of patients who may not recover their sense of smell or taste, based on existing trajectories of recovery. The results were alarming, with approximately 5 per cent of COVID-19 patients with initial smell or taste loss having persistent abnormalities.
To provide a more personal perspective on the effects of losing one's sense of smell, the team worked with AbScent, a charity in the United Kingdom, to interview patients who had lost their sense of smell for over a year. "It made all the numbers come alive," Benjamin recalls.
The study was published in the British Medical Journal (BMJ), one of the four most prestigious scientific journals in medicine, and garnered significant attention from over 200 news outlets worldwide.
In another research project with Assistant Professor Raghav Sundar, who is also a gastrointestinal oncologist at the National University Cancer Institute, Benjamin explored the efficacy of immunotherapy treatments on gastric cancer.
 Benjamin (left) taking a selfie with Prof Raghav.
Benjamin (left) taking a selfie with Prof Raghav.
His team developed a method to reconstruct data that was previously unpublished by pharmaceutical companies, and discovered that a portion of gastric cancer patients actually fared worse on expensive immunotherapy drugs as compared to conventional chemotherapy.
The team's findings, published in the world-leading Journal of Clinical Oncology, were immediately practice-changing, and they made their method publicly available. Other researchers have since used their technique on various other cancers, including oesophageal and head and neck cancers.
Benjamin credits Prof Raghav for the past four years of unwavering mentorship through the full breadth of medical research — teaching him how to write clinical trial protocols and manuscripts, obtain ethics approval, while encouraging him to attend conferences and helping him secure funding for his research.
Building a community of carers
School has not been the only thing on Benjamin’s mind: he has also been a tireless advocate of the social impact medical students can enact. With NUS’ support, he has been able to combine his interests in medicine, research and public service to create meaningful change.
One of Benjamin's significant projects was leading the Neighbourhood Health Service (NHS), a student-led, school-supported initiative focused on providing free health screenings and follow-up care to low-income residents living in rental flats, for which he served as Co-Director.
Looking back, Benjamin credits much of his success to the guidance and mentorship of Professors Gerald Koh and Tay Sook Muay, who inspired him and guided him through challenging situations with finesse.
"I'm thankful to be part of a school that promotes student-led community service," Benjamin says. "At the NHS events, my classmates and I stepped into the homes of low-income seniors to see how socio-economic and psychological factors impacted their access to healthcare. It was a humbling experience for many of us who grew up relatively free from hardship."
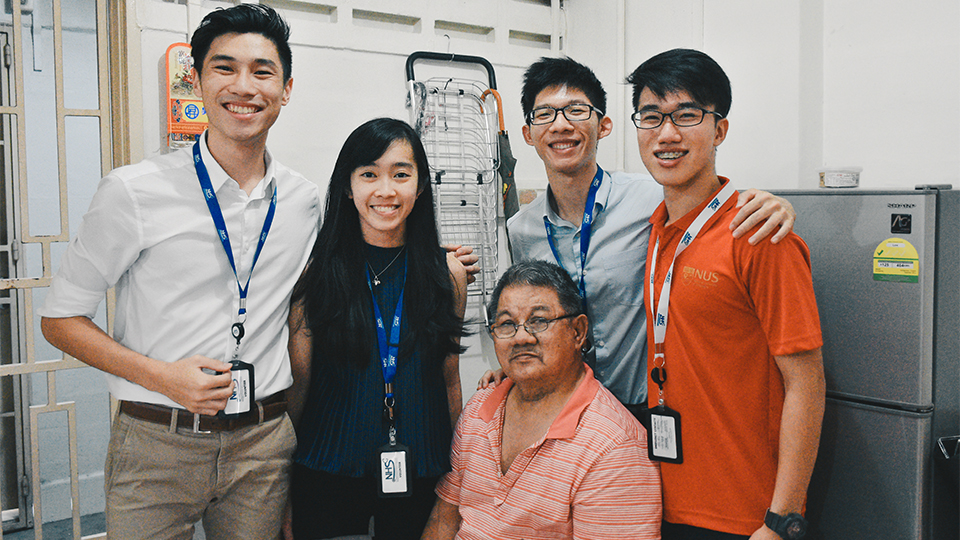 Benjamin (standing, first from right) and other Neighbourhood Health Service volunteers visiting a senior in his flat to provide follow-up care.
Benjamin (standing, first from right) and other Neighbourhood Health Service volunteers visiting a senior in his flat to provide follow-up care.
A world of opportunities
Benjamin was also able to seize a learning opportunity prior to the pandemic, when he chaired the planning of an exchange with Tzu Chi University in Hualien, Taiwan to participate in their “silent mentor” or body donor programme. There, he was able to learn from the cadavers of people who selflessly donated their bodies for medical research and education, develop compassion and empathy, and aspire to become a humane doctor after graduation.
 Benjamin (eighth from left) with fellow students from NUS Medicine visiting the Gedusang Music Studio in Jiamin Village, Hualien County during their Taiwan exchange to learn about its aboriginal people and their music.
Benjamin (eighth from left) with fellow students from NUS Medicine visiting the Gedusang Music Studio in Jiamin Village, Hualien County during their Taiwan exchange to learn about its aboriginal people and their music.
Reflections of an on-call doctor
As a junior doctor, Benjamin has learned not to be too hard on himself. “We do 36-hour calls — that means going to work at 6am today and leaving work at about 1pm the next day — at least once or twice a week. It’s gruelling, and you’d be lucky to get an hour or two of sleep overnight,” he shares. He is thankful to his patients and colleagues who keep him going, and his family for their understanding. Benjamin also sees great value in humility and believes there is always an opportunity to learn from everyone, including patients and their families.
He suggests for aspiring medical students to get involved in healthcare, whether through job shadowing at clinics and hospitals, or volunteering at senior activity centres or hospices, to find out if they might like medicine.
He also offers reassurance to current medical students:
"When the going gets tough, remember that you are not alone and that your seniors are happy to support and guide you through this journey. You don’t have to face your challenges alone!”
 Benjamin (centre) and his study buddies Chai Yi Xuen and Abraham Sui at Commencement 2022.
Benjamin (centre) and his study buddies Chai Yi Xuen and Abraham Sui at Commencement 2022.